Introduction
In recent decades, assisted reproductive technologies (ART) have revolutionized the field of reproductive medicine, offering hope to millions of individuals and couples facing fertility challenges. As societal norms shift and family structures evolve, the demand for ART continues to grow, encompassing a wide range of treatments from in vitro fertilization (IVF) to more advanced genetic interventions.
This comprehensive guide aims to demystify the science and process behind ART, offering readers—whether prospective patients, healthcare professionals, or curious minds—a well-rounded understanding of the landscape. We’ll explore the emotional, ethical, and scientific dimensions of these technologies, while also addressing disparities in access and recent innovations that promise to shape the future of reproductive health.
Whether you’re at the beginning of your fertility journey, a practitioner guiding patients through complex choices, or simply intrigued by how far medical science has come, this article is designed to inform, support, and inspire.
Understanding Assisted Reproductive Technologies
Assisted reproductive technologies (ART) encompass a spectrum of medical procedures used primarily to address infertility. These technologies assist in achieving pregnancy through means other than sexual intercourse and have become a cornerstone of modern fertility treatment.
What is ART?
ART includes all fertility treatments in which either eggs or embryos are handled outside the body. The most commonly known form is in vitro fertilization (IVF), but ART also includes procedures such as intracytoplasmic sperm injection (ICSI), egg and sperm donation, gestational surrogacy, and cryopreservation of gametes and embryos.
History and Evolution
The roots of ART can be traced back to the late 19th century, but it wasn’t until 1978 that the first baby was born through IVF in the United Kingdom. Since then, the field has expanded exponentially, benefiting from advances in microscopy, endocrinology, and molecular genetics. ART has evolved from experimental procedures to widely accepted medical practices that are now available in clinics worldwide.
Key Concepts and Terminology
Understanding ART requires familiarity with certain key terms:
- Ovulation induction: Stimulating a woman’s ovaries to produce multiple eggs.
- Egg retrieval: A procedure to collect mature eggs from the ovaries.
- Fertilization: Combining eggs and sperm, either naturally (in vitro) or through techniques like ICSI.
- Embryo transfer: Placing the resulting embryo(s) into the uterus.
- Cryopreservation: Freezing eggs, sperm, or embryos for future use.
Each of these steps involves careful medical coordination and carries its own set of considerations and potential complications.
By grasping these foundational concepts, readers can better understand the specific procedures and decisions involved in ART, setting the stage for deeper exploration in the sections to follow.
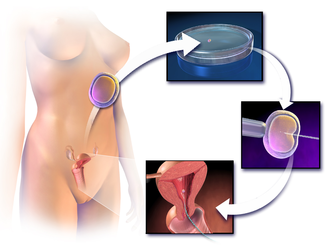
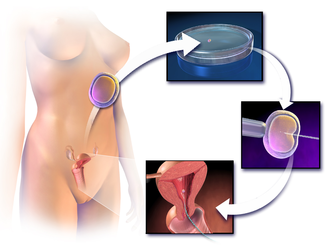
In Vitro Fertilization (IVF): The Cornerstone of ART
In vitro fertilization (IVF) is the most widely recognized and commonly performed assisted reproductive technology. It involves retrieving mature eggs from the ovaries, fertilizing them with sperm in a laboratory, and transferring one or more resulting embryos into the uterus. Since the birth of the first IVF baby in 1978, over 8 million babies have been born worldwide through this method.
The IVF Process: Step by Step
- Ovarian stimulation: Hormonal medications are used to stimulate the ovaries to produce multiple eggs.
- Monitoring and egg retrieval: Through ultrasound and blood tests, follicle development is tracked. Eggs are retrieved via a minor surgical procedure.
- Fertilization and embryo culture: Eggs are combined with sperm in the lab. Fertilization may occur naturally or via ICSI. Fertilized eggs (embryos) are cultured for several days.
- Embryo transfer: A selected embryo is transferred into the uterus, typically on day 3 or 5 post-fertilization.
- Luteal phase support and pregnancy test: Hormonal support continues after transfer, and a pregnancy test is conducted approximately two weeks later.
Success Rates and Influencing Factors
IVF success rates vary depending on numerous factors:
- Age of the individual: Younger individuals typically have higher success rates.
- Cause of infertility: Certain conditions may reduce the likelihood of success.
- Embryo quality: Affected by egg and sperm health, lab conditions, and timing.
- Clinic experience and technology: Outcomes can vary widely between clinics.
While success rates have improved significantly, IVF is not guaranteed, and multiple cycles may be necessary.
Common Misconceptions
- “IVF always works on the first try”: Many patients require more than one cycle.
- “Only older individuals use IVF”: IVF is used for various fertility challenges, regardless of age.
- “IVF guarantees twins or triplets”: With modern single embryo transfer (SET), the risk of multiples has decreased.
Understanding the complexities and realities of IVF helps set accurate expectations for patients and can guide more informed decisions. As a foundational technique in ART, IVF continues to evolve with technological advancements, making it more effective, safer, and accessible than ever before.
Emotional and Psychological Aspects
The journey through assisted reproductive technologies can be emotionally taxing, marked by highs of hope and lows of disappointment. For many individuals and couples, fertility challenges strike at the core of identity, relationships, and life plans.
The Emotional Landscape of ART
Undergoing ART is not just a medical experience—it is also a deeply emotional one. People may experience a range of feelings:
- Hope and excitement about the possibility of conceiving
- Stress and anxiety related to medical procedures and uncertainty
- Grief and loss following unsuccessful cycles or miscarriages
- Isolation and stigma, particularly for those without a strong support network
These emotions can be cyclical and unpredictable, often intensified by the hormonal medications used during treatment.
Impact on Relationships
Fertility treatments can affect both partners in a relationship, potentially creating emotional distance or fostering greater intimacy. Common challenges include:
- Communication breakdowns
- Differing coping mechanisms and expectations
- Financial stress due to the high cost of treatment
It’s important for couples to seek open dialogue and professional support when needed. Individual or couples counseling can help address these issues and strengthen the relationship.
The Role of Counseling and Support
Many fertility clinics now offer integrated psychological services, recognizing the mental health challenges ART can present. Counseling provides a space to process emotions, reduce anxiety, and build resilience.
Support groups—both online and in-person—also offer valuable opportunities to connect with others going through similar experiences. Shared stories can reduce feelings of isolation and create a sense of community.
Cultural and Social Considerations
Cultural expectations and societal pressures around parenthood can further complicate the emotional journey. In some cultures, infertility may carry stigma, leading individuals to pursue ART in secrecy. Others may face judgment based on age, marital status, or sexual orientation.
Recognizing these social factors is crucial in providing compassionate and holistic care. Emotional wellbeing should be seen as a core part of fertility treatment—not an optional add-on.
By acknowledging and addressing the psychological dimensions of ART, individuals and healthcare providers can better navigate the emotional complexity of fertility treatment and promote overall well-being.
In the next section, we will explore the accessibility and affordability of ART, examining how systems and structures influence who gets to benefit from these life-changing technologies.
Accessibility and Affordability of ART
Despite the life-changing potential of assisted reproductive technologies, access to these services remains highly unequal. Socioeconomic, geographic, legal, and cultural barriers often determine who can benefit from ART—and who cannot. Addressing these disparities is essential to creating a more equitable reproductive healthcare system.
Global Disparities in Access
Availability of ART varies dramatically around the world. In some countries, particularly in parts of Europe and Asia, ART is widely accessible through public healthcare systems or regulated private sectors. In others—especially in low- and middle-income regions—access is limited or non-existent due to cost, infrastructure, or restrictive laws.
- High-income countries: ART may be subsidized or covered by insurance, but access can still depend on factors like age limits or number of allowable cycles.
- Low-income countries: Clinics may be scarce, and treatments often remain financially out of reach, with little government support.
- Legal restrictions: Laws governing ART differ widely, affecting who can access treatment (e.g., single individuals, same-sex couples) and under what conditions.
These disparities contribute to global “reproductive tourism,” where individuals travel to access services unavailable or unaffordable in their home countries—raising ethical concerns around regulation, consent, and exploitation.
Cost and Insurance Coverage
The high cost of ART is one of the biggest barriers to access. A single IVF cycle can cost thousands to tens of thousands of dollars, with additional costs for medications, testing, cryopreservation, and more. Most patients require more than one cycle to achieve pregnancy.
Insurance coverage is inconsistent:
- United States: Only some states mandate insurance coverage for infertility treatments, and coverage varies by employer and plan.
- Europe and Canada: Many countries offer partial or full public coverage for ART, though often with eligibility criteria.
- Private financing: In the absence of public or insurance support, many patients rely on loans, savings, or crowdfunding.
The financial burden can lead to emotional stress, medical debt, and difficult decisions about continuing treatment.
Social and Cultural Barriers
Even where ART is technically available, social and cultural factors can restrict access:
- Stigma and misinformation: Cultural taboos around infertility or assisted reproduction may deter individuals from seeking care.
- Discrimination: Some providers may refuse treatment to individuals based on marital status, sexual orientation, age, or disability.
- Language and literacy barriers: Complex procedures and consent forms may be inaccessible to those with limited health literacy or language proficiency.
Culturally sensitive care and community education are essential to breaking down these barriers and ensuring ART is accessible to all who need it.
Improving Equity in ART
Efforts to improve accessibility must address both systemic and individual-level challenges:
- Policy reforms: Expanding public funding and mandating insurance coverage can significantly increase access.
- Clinic-level initiatives: Sliding scale fees, financial counseling, and outreach to underserved populations help reduce financial and social barriers.
- Technological innovation: Simplifying and reducing the cost of ART procedures—such as low-cost IVF protocols—can make treatment more affordable globally.
By addressing the affordability and accessibility of ART, we take a critical step toward reproductive justice—the idea that everyone should have the right and means to build a family if and when they choose.
In the next section, we’ll explore the latest advancements in assisted reproductive technologies and how they are transforming the future of fertility care.
Accessibility and Global Disparities
While assisted reproductive technologies (ART) have advanced significantly in recent years, the reality is that access to these services is not universal. Factors such as financial barriers, insurance coverage, availability across different countries, and cultural or religious perspectives significantly influence who can benefit from ART. These disparities present significant challenges, with millions of people across the world facing obstacles to accessing the fertility treatments they need.
Financial Barriers and Insurance Coverage
One of the most pressing barriers to ART is the cost. The price of treatments such as in vitro fertilization (IVF), intrauterine insemination (IUI), or sperm and egg donation can be prohibitively high, often reaching tens of thousands of dollars per cycle. Many individuals and couples face the harsh reality that they cannot afford to pursue these life-changing treatments without significant financial strain. This is especially true for patients who need multiple cycles or additional services like genetic testing, embryo freezing, or hormonal therapies.
In many countries, the lack of insurance coverage for ART exacerbates this issue. While some nations offer fertility treatments as part of public health coverage, in other regions, these procedures are considered elective and are therefore not covered by government-funded health plans. Even private insurance may exclude ART from its coverage due to its high cost and the fact that fertility treatments are not always considered “medically necessary” under traditional definitions of health care.
For people who are uninsured or underinsured, the financial burden of ART can force them to make difficult decisions, including choosing less effective treatments, delaying treatment, or abandoning their fertility journey altogether. Some countries have recognized the importance of ART and have started to implement policies that support coverage, but much more needs to be done to ensure equitable access to these services.
Availability Across Different Countries
Access to ART varies dramatically from one country to another. In countries with advanced healthcare systems, ART is widely available and supported by highly trained specialists and cutting-edge medical technology. However, in many parts of the world, access to ART is limited or non-existent. This disparity is often rooted in differences in national healthcare systems, economic resources, and infrastructure.
- Developed countries: In nations like the United States, Canada, the United Kingdom, and many parts of Europe, ART is generally accessible, although financial barriers still exist due to the cost of treatment and insurance limitations. These countries typically have well-established clinics and a high level of medical expertise, making ART a feasible option for many people.
- Developing countries: In many low- and middle-income countries, ART is either unavailable or prohibitively expensive. Healthcare infrastructure may be insufficient to support the advanced technology required for fertility treatments, and a lack of trained medical professionals may limit the availability of ART options. As a result, individuals seeking ART often have to travel to wealthier countries, a practice known as “reproductive tourism.”
- Emerging markets: Some countries in Asia, Africa, and Latin America are seeing a growing demand for ART and are making strides in improving access. For example, India and Thailand have become popular destinations for international patients seeking affordable ART treatments. However, even in these regions, disparities in access persist, particularly for local populations who may not have the financial means to take advantage of these services.
Cultural and Religious Perspectives
Cultural and religious beliefs play a significant role in shaping attitudes toward ART. In some cultures, infertility is viewed as a deeply personal issue that may carry social stigma, making it difficult for individuals to openly seek ART services. In other societies, the use of ART may be embraced as a means of overcoming fertility challenges and fulfilling family expectations. However, there are cultural and religious perspectives that actively oppose or limit the use of ART.
- Religious opposition: Certain religious groups object to aspects of ART based on doctrinal beliefs. For example, some Christians, Muslims, and Catholics believe that ART treatments like IVF may interfere with divine will or the natural order of conception. Concerns may also arise regarding the use of donor sperm or eggs, or the creation and disposal of embryos. These religious objections can lead to restrictions on the use of ART in some countries, particularly where religious influence is strong in public policy.
- Cultural perceptions: In cultures with strong emphasis on family lineage and reproduction, ART can be seen as both a medical and a social necessity. In countries like Japan and South Korea, where population decline and aging demographics are pressing issues, ART is encouraged as a means of preserving family structures. However, in some parts of the world, traditional views of fertility, gender roles, and family might conflict with the practices involved in ART. For example, the notion of surrogacy may be taboo in certain regions, and egg donation may be seen as unethical or even immoral.
- Social stigma: Individuals and couples seeking ART often face societal stigma, especially in countries or cultures where infertility is considered a private or shameful issue. This stigma can discourage people from seeking the help they need, further exacerbating the challenges they face. Societal pressures related to childbearing and reproductive success may also impact mental health and emotional wellbeing, adding to the complexities of the ART journey.
The Need for Global Dialogue and Policy Reform
As ART technologies continue to evolve, there is an urgent need for a global dialogue about the accessibility and regulation of these treatments. Policymakers must work to ensure that ART is not restricted by financial, geographic, cultural, or religious barriers. Efforts to improve access could include:
- Increased insurance coverage: Expanding insurance coverage for ART is a critical step in making these treatments more affordable for a broader population.
- Regulation and standardization: Ensuring that ART is regulated in a way that promotes safety, quality, and ethical practice, while allowing for flexibility in how treatments are delivered.
- Cross-border cooperation: Encouraging collaboration between countries to share knowledge, improve healthcare infrastructure, and reduce inequalities in access to reproductive technologies.
- Cultural sensitivity: Recognizing and respecting cultural and religious differences while striving to create policies that uphold the right to fertility treatment for all individuals.
Access to ART is not just a medical or technological issue—it is a social and ethical one. As the field of reproductive medicine continues to expand, it is essential that efforts to make ART accessible are inclusive, equitable, and culturally sensitive, ensuring that no one is left behind in the quest for parenthood.
Choosing the Right Clinic and Team
Choosing the right clinic and medical team is one of the most important decisions in the assisted reproductive technology (ART) journey. With so many factors to consider, from success rates to the comfort level of the clinic’s staff, this decision can feel overwhelming. However, making an informed choice can significantly influence your experience and outcomes. Below, we’ll explore key considerations to help guide your selection process.
1. Success Rates
Success rates are often one of the first things prospective patients look at when choosing a clinic. These statistics give an indication of how many patients successfully achieve pregnancy through ART at a particular clinic. However, it’s important to interpret success rates with caution:
- Age-specific rates: Clinics may publish overall success rates, but it’s crucial to look at success rates broken down by age group, as fertility treatments tend to be more successful for younger individuals.
- Cause of infertility: Clinics may have different success rates depending on the type of infertility being treated, such as male factor infertility, female age-related infertility, or unexplained infertility.
- Multiple cycles: Consider how many cycles patients typically undergo before achieving success. A clinic with high success rates may also have a higher number of failed attempts, which could indicate a more aggressive treatment approach.
Success rates are an important factor, but they should be balanced with other considerations, such as the clinic’s reputation, staff, and your own comfort level with the process.
2. Experience and Qualifications of the Medical Team
The qualifications and experience of the medical team are essential in ensuring the best care. Fertility specialists should have the appropriate certifications, such as board certifications in obstetrics and gynecology or reproductive endocrinology. Here’s what to look for:
- Fertility specialists: Look for a team with a board-certified reproductive endocrinologist who specializes in ART procedures. This specialist should have experience in treating the specific fertility challenges you are facing.
- Embryologists: The role of embryologists is critical in ART, as they handle the fertilization process and embryo culture. Check if the clinic employs certified embryologists with significant experience.
- Nurses and counselors: Nurses should be knowledgeable about the procedures and medications, while counselors can provide vital emotional support. A compassionate, well-trained support staff can make a big difference in your experience.
It’s important to feel comfortable and confident in the abilities of your medical team. Don’t hesitate to ask about their experience, education, and specific success stories related to your type of treatment.
3. Clinic Reputation and Reviews
Word-of-mouth, online reviews, and referrals from healthcare providers can be invaluable when choosing an ART clinic. While online reviews can sometimes be subjective, there are several ways to evaluate a clinic’s reputation:
- Patient testimonials: Look for testimonials from patients who have undergone similar treatments. Positive experiences can provide insight into the clinic’s level of care, professionalism, and patient support.
- Professional reputation: Check if the clinic is affiliated with reputable organizations, such as the American Society for Reproductive Medicine (ASRM) or the European Society of Human Reproduction and Embryology (ESHRE). These affiliations ensure the clinic adheres to industry standards.
- Word-of-mouth referrals: Speak with others who have undergone ART. Personal recommendations can offer a more balanced perspective and may help you discover hidden gems that are not as widely advertised.
Ultimately, the clinic’s reputation in your community and beyond will give you confidence in their abilities.
4. Treatment Options and Specialties
Different clinics offer different ART procedures, and some may have specific expertise in certain areas. It’s important to select a clinic that provides the treatment options you may need, such as:
- IVF and ICSI: If in vitro fertilization (IVF) is the best option for you, confirm that the clinic offers IVF and related services like intracytoplasmic sperm injection (ICSI).
- Egg freezing and sperm banking: If you’re considering fertility preservation, ensure that the clinic offers cryopreservation services, including egg, sperm, and embryo freezing.
- Genetic testing: Clinics offering preimplantation genetic testing (PGT) or genetic screening can be critical if you’re at risk for genetic disorders or if you’re using donor eggs or sperm.
- Fertility preservation for cancer patients: Some clinics specialize in fertility preservation for cancer patients undergoing chemotherapy or radiation, so consider their experience in this area if applicable.
By choosing a clinic that specializes in the treatment options you require, you can feel confident that the clinic has the necessary resources and expertise to manage your specific needs.
5. Clinic Environment and Facilities
The physical environment of the clinic is an often-overlooked but critical aspect of choosing the right fertility center. The clinic should have a clean, modern, and comfortable setting that fosters a sense of trust and security. When touring potential clinics, pay attention to:
- Cleanliness and comfort: A well-maintained clinic with clean, modern facilities can signal the clinic’s attention to detail and its commitment to patient safety.
- Technology and equipment: Advanced technology and cutting-edge equipment are essential for ART procedures. Ensure the clinic is equipped with the latest medical devices, such as ultrasound machines, incubators, and genetic testing tools.
- Private, welcoming atmosphere: Fertility treatments can be emotionally challenging, so a clinic that offers private spaces for consultations, as well as a welcoming and supportive atmosphere, can help ease the process.
Visiting the clinic in person (if possible) and observing the facilities can provide valuable insight into what your experience might be like.
6. Communication and Support
Effective communication with your clinic’s team is essential throughout the ART process. From the initial consultation to the final stages of treatment, you should feel comfortable asking questions and expressing concerns. Consider the following when evaluating a clinic’s communication:
- Accessibility: Can you easily get in touch with your doctor or support staff? Are they responsive to emails, phone calls, and texts?
- Information clarity: Does the clinic provide clear, understandable information about procedures, costs, and expectations? This can include written materials, online resources, and detailed explanations during consultations.
- Emotional support: Fertility treatments can be emotionally challenging, so it’s essential that the clinic offers counseling services or has partnerships with mental health professionals who specialize in fertility. A clinic that understands the emotional toll of ART can provide significant value beyond medical care.
Feeling comfortable and supported by the clinic’s team is vital to navigating the ups and downs of ART.
7. Cost and Transparency
The cost of ART varies widely, depending on the clinic and the treatments involved. Ensure that the clinic provides clear, upfront pricing, including any potential additional costs for medications, procedures, and follow-up care. Some things to consider:
- Cost breakdown: Ask for a detailed breakdown of all the costs involved in treatment. Some clinics may provide package deals that include multiple cycles, while others may charge per cycle.
- Financing options: Inquire if the clinic offers financing or payment plans to help manage the financial burden of ART.
- Insurance coverage: Verify if the clinic works with your insurance provider, or if they can offer guidance on seeking insurance reimbursement for ART procedures.
Cost transparency ensures that you’re not blindsided by hidden fees and can help you make a more informed decision.
Conclusion: Trust and Comfort
Ultimately, choosing the right ART clinic and team is about finding a place where you feel both comfortable and confident. The clinic you select should offer the expertise and resources necessary to support your fertility journey while providing a compassionate, patient-centered experience. By evaluating success rates, medical expertise, reputation, facilities, communication, and cost, you can make a decision that aligns with your needs and values, setting you on the path to achieving your reproductive goals.
In the next section, we will explore the future of ART and emerging technologies that are shaping the landscape of fertility treatments.
References
- For further reading, explore ASRM guidelines 1, RESOLVE support networks 8, and IFFS global reports 1.